Abstract
Introduction: CMML is a myeloid neoplasm hallmarked by cytopenias and a peripheral monocytosis. Although uniformly fatal, many patients (pts) are diagnosed incidentally and are monitored without treatment. Therapy is implemented when symptomatic cytopenias, splenomegaly, or bone marrow progression occur. Higher white blood cell count (WBC) and absolute monocyte count (AMC) are associated with inferior OS, however, they are currently not an indication for treatment. Case reports have demonstrated a putative link between CMML monocytes and end organ damage (EOD), which has not been systematically explored. We hypothesize that CMML cases with higher WBC and/or AMC will be at increased risk for EOD and that cytoreductive therapy could mitigate this risk.
Methods: CMML pts with at least 2 measures of creatinine and liver function tests were retrospectively identified from the Moffitt Cancer Center CMML database. EOD was defined as the interval development of chronic kidney disease (CKD), acute kidney insufficiency (AKI) by Kdigo criteria, liver dysfunction, pleural effusion, or cardio-vascular events (CVE). CKD was defined by a GFR<60 for greater than 3 months. Those pts with preexisting EOD, to include CKD or history of AKI, transformation to Acute Myeloid Leukemia, or allogeneic transplant were excluded from this study. Categorical variables were compared with the Fisher's exact test and quantitative variables compared utilizing the Mann-Whitney test. The Kaplan-Meier method and log-rank test were used to estimate overall survival (OS).
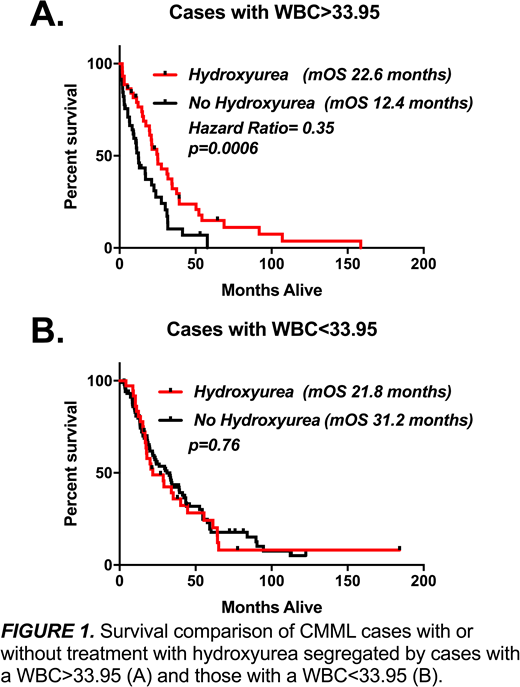
Results: Between 1/1/2000 and 1/1/2018, 313 CMML cases were identified that met the above criteria for study entry. The median age of pts in this cohort was 70 (31-95 range) with a male predominance (66%). 168 pts were classified as WHO CMML-0 (54%), 78 as CMML-1 (25%), and 67 as CMML-2 (21%). The majority of cases were intermediate risk by the Global MDACC score (30% INT-1, 28% INT-2). The most common somatic mutations included TET2(64%), ASXL1(44%), and SRSF2(45%). AKI was the most common type of EOD that occurred in 37% of cases, with new CKD in 8.6% of pts. Pleural effusions, defined by radiographic evidence by X-ray or CT-scan occurred in 29% of cases. Liver dysfunction, defined as transaminitis or hyperbilirubinemia 1.5x the upper limit of normal, occurred in 14% of cases, and CVE were recorded in 4.5% of cases. Development of new CKD (9.2% v 1.2%, p=0.012) and liver dysfunction (13.2% v 3.5%, p=0.012) were significantly more common in myeloproliferative-CMML (MPN) defined by FAB criteria. Because the FAB criteria relies solely on WBC, we explored the impact of WBC and AMC on EOD. To account for variability of longitudinal measures, we isolated the patient-specific peak WBC and AMC along with the corresponding markers of EOD for each peak, respectively. Using these variables WBC (Spearman r-value 0.25, p<0.0001), and to a greater extent AMC (Spearman r-value 0.30, p<0.0001), linearly correlated with creatinine and were associated with AKI (median AMC 11.7 vs. 5.5, p< 0.0001; median WBC 54.7 vs. 35.6, p <0.0001) and CKD (median AMC 19.7 vs. 6.5, p = 0.0002; median WBC 73.1 vs. 40.7, p = 0.002). This association remained significant when combining all EOD events (median AMC 11.4 vs 4.5, p <0.0001; median WBC 54.4 vs. 29, p < 0.0001). To identify a WBC and AMC within MPN-CMML that could be targeted for therapeutic intervention, we divided our cohort into WBC and AMC quartiles. Importantly, only the first quartile, defined by an upper boundary of 33.95 cells/dL for peak-WBC and 5.4 cells/dL for peak-AMC was statistically associated with a lower creatinine (p<0.004), AKI (p<0.0008), CKD (p<0.0003), or combined EOD events (p<0.002). MPN-CMML pts with new AKI had an inferior OS (17.1m v 30.7m, HR=1.51, p=0.0007) as did patients with a baseline WBC >33.95 (19.8m v 29.6m, p = 0.004). Patients with a baseline WBC at diagnosis >33.95 cells/dL treated with hydroxyurea had improved overall survival (22.6m vs. 12.4m, HR 0.35, p= 0.0006). This survival advantage did not hold in CMML patients with baseline WBC lower than 33.95 cells/dL suggesting that treatment may only mitigate poor outcomes in high WBC CMML patients (Figure 1).
Conclusions: MPN-CMML is associated with EOD that includes AKI/CKD, pleural effusions, LFT abnormalities, and CVE. Those cases with a WBC >33.95cells/dL are at particularly high risk for EOD and cytoreductive therapy should be routinely considered to mitigate this risk.
Sweet:Celgene: Honoraria, Speakers Bureau; Phizer: Consultancy; BMS: Honoraria; Agios: Consultancy; Astellas: Consultancy; Jazz: Speakers Bureau; Jazz: Speakers Bureau; Novartis: Consultancy, Honoraria, Speakers Bureau; Novartis: Consultancy, Honoraria, Speakers Bureau; BMS: Honoraria; Phizer: Consultancy; Agios: Consultancy; Astellas: Consultancy; Celgene: Honoraria, Speakers Bureau. Sallman:Celgene: Research Funding, Speakers Bureau. List:Celgene: Research Funding. Komrokji:Novartis: Honoraria, Speakers Bureau; Novartis: Honoraria, Speakers Bureau; Novartis: Honoraria, Speakers Bureau; Celgene: Honoraria, Research Funding; Celgene: Honoraria, Research Funding; Novartis: Honoraria, Speakers Bureau.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal